Exploring Innovative Solutions to Ease Budget Constraints in Rural and Small Hospitals
In rural and small hospitals, intensive care units (ICUs) often face unique challenges, particularly when it comes to budget constraints. These facilities may struggle to maintain adequate staffing, equipment, and resources necessary to provide high-quality critical care services. However, amidst these challenges, several innovative ICU solutions have emerged to help alleviate financial burdens and ensure patients in these communities receive the care they need. One such solution gaining traction is the implementation of tele-ICU services.
Tele-ICU: Bridging Gaps in Critical Care
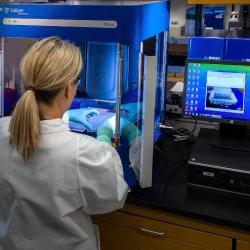
Tele-ICU, also known as remote monitoring or virtual ICU, utilizes advanced technology to connect ICU patients in rural and small hospitals with critical care specialists located off-site. Through real-time audio and video communication, specialists can remotely monitor patients, review vital signs, and collaborate with on-site staff to provide timely interventions.
One of the primary benefits of tele-ICU is its ability to extend the expertise of critical care specialists to facilities that may not have access to such resources locally. This not only improves patient outcomes but also enhances staff confidence and reduces the need for patient transfers to larger medical centers.
Cost-Effective Solutions for Rural Hospitals
Apart from tele-ICU, several other cost-effective solutions exist to address budget constraints in rural and small hospital ICUs:
- Remote Monitoring Technologies: Remote monitoring devices allow for continuous tracking of patients' vital signs and other parameters, alerting staff to any deviations from normal values. These technologies can help prevent adverse events and reduce the need for constant bedside supervision, thereby optimizing staff utilization and minimizing costs.
- Collaborative Care Models: Collaborative care models involve partnerships between rural hospitals and larger medical centers, enabling the sharing of resources, expertise, and best practices. By leveraging economies of scale and pooling resources, participating hospitals can reduce expenses while maintaining high standards of care.
- Staff Training and Education Programs: Investing in staff training and education programs is crucial for ensuring competency and proficiency among ICU personnel. By providing ongoing education opportunities, hospitals can empower their staff to deliver quality care effectively, thus reducing the likelihood of costly errors or complications.
- Utilization of Telemedicine for Consultations: Telemedicine platforms can facilitate remote consultations with specialists in various medical disciplines, allowing rural hospitals to access expert advice without the need for physical presence. This not only enhances patient care but also reduces the financial burden associated with transporting patients or seeking external consultations.
- Resource Sharing Networks: Establishing networks for sharing equipment, supplies, and personnel among neighboring hospitals can help optimize resource allocation and reduce overhead costs. By collaborating with nearby facilities, rural hospitals can ensure access to essential resources while minimizing unnecessary expenditures.
Looking Ahead: Embracing Innovation for Sustainable Healthcare
As healthcare providers continue to navigate budget constraints in rural and small hospital ICUs, embracing innovation will be paramount to ensuring sustainable and high-quality care delivery. Tele-ICU services, alongside other cost-effective solutions such as remote monitoring technologies, collaborative care models, staff training programs, telemedicine, and resource sharing networks, offer promising avenues for addressing financial challenges while prioritizing patient outcomes.
Conclusion
By leveraging these innovative solutions and fostering partnerships within the healthcare community, rural hospitals can overcome budget constraints and fulfill their mission of providing accessible, comprehensive, and compassionate care to patients in underserved areas.
More to Read:
Previous Posts: