How Nursing Informatics Is Improving Patient Outcomes

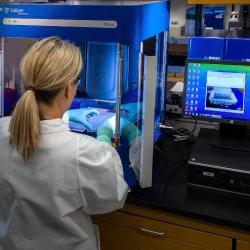
Nursing informatics is a dynamic and evolving field, combining nursing science and information technology to harness the power of digital tools. This includes the strategic application of electronic health records (EHRs), clinical decision support systems, telehealth solutions, and other technological advancements to enhance nursing practice and ultimately improve patient outcomes.
The integration of technology in healthcare is essential for streamlining workflows and boosting efficiency, but also for elevating the quality of care delivered to patients. Using computerized systems for patient data management, nursing informatics has evolved throughout the decades. It empowers nurses to make informed decisions and collaborate effectively and is shaping the future of healthcare delivery.
Enhancing patient safety and quality of care through technology
In healthcare, technology is a powerful tool for enhancing patient safety and care quality. Electronic health records and clinical decision support systems (CDSS) play a pivotal role.
EHRs replace manual record keeping, providing nurses with instant access to accurate patient data, reducing errors, and streamlining workflows. CDSS uses algorithms and evidence-based guidelines to provide real-time recommendations to medical personnel, assisting in identifying problems and finding solutions. It can inform nurses about drug interactions, suggest diagnostics, and align treatments with existing protocols.
These technologies work with healthcare's commitment to safety and quality by empowering nurses with accurate information and decision-making support. This interaction between technology and human expertise ensures high standards of care.
Rather than solely relying on technology, nurses are encouraged to treat it like any other nursing tool to back up their knowledge gained from qualifications such as a nursing leadership degree. Baylor University offers the Doctor or Nursing Practice (DNP) program, which can be studied online. This arms healthcare leaders with advanced tech and data-related skills and knowledge to bring back to their healthcare organization and improve patient care.
Encouraging communication and collaboration
In healthcare, efficient communication and collaboration among different teams are essential for delivering the best care to patients. Technology makes this possible through interoperability and data sharing. Patient information is shared seamlessly among various providers, enhancing care coordination.
Telehealth has also transformed communication and consultation. It uses video conferencing and wearable devices to bridge gaps in care, particularly in remote areas. Nurses use telehealth for remote patient monitoring and engaging in real-time consultations. This reduces the time and cost of traveling and the risks associated with waiting with other potentially sick patients. For someone who may have a reduced immune system, this prevents their health from worsening.
This technology also enhances patient care. People are more likely to attend a remote appointment that takes just minutes of their time than an in-person appointment they have to go out of their way to attend.
The benefits of electronic health records
EHRs have changed how healthcare information is documented, accessed, and managed. This benefits nurses and patients, with enhanced accuracy and care coordination. For nurses, EHRs reduce manual efforts, enabling quicker input, retrieval, and updates of patient data, meaning they can focus more on direct care and informed decision making. Patients benefit from this improvement in the quality of care. EHRs replace illegible notes, reducing errors and enabling real-time data access.
The benefits of clinical decision support systems
CDSS taps into medical knowledge, research, and data analytics to provide nurses with relevant insights at the point of care. This empowers nurses to make informed choices in the moment. It can also protect against errors. For example, it can generate alerts for drug interactions and allergies. In an emergency situation, this helps the patient receive safe and effective treatment much quicker.
Customization allows nurses to tailor CDSS to specific clinical scenarios, patient characteristics, and treatment plans, creating a responsive and personalized decision support system. This amplifies nursing decision making, streamlines workflows, and cultivates patient-centred care. By seamlessly incorporating CDSS into their practice, nurses navigate the intricacies of patient care with increased assurance and efficacy.
Information exchange and interoperability
Health information exchange (HIE) enables seamless sharing of vital medical information among different providers and facilities, helping with informed decision making and care coordination. This interconnectedness ensures that healthcare professionals have access to a patient's complete medical history, diagnoses, treatments, and test results. This shared information prevents redundant tests, minimizes medical errors, and optimizes treatment planning, ultimately enhancing patient outcomes.
Remote monitoring through devices
Wearable devices can be used to collect a continuous stream of patient health data. These remote patient monitoring (RPM) devices, ranging from smartwatches to wearable sensors, monitor vital signs, activity levels, and other relevant metrics. By gathering this information, RPMs offer a comprehensive view of a patient's health status, enabling healthcare providers to monitor chronic conditions remotely. Previously, a patient would have needed to stay in a hospital for one or more days to be monitored.
The real-time data collected through RPMs allow for the early detection of subtle changes in a patient's health. Deviations from established patterns can trigger alerts for healthcare professionals, allowing for timely interventions. This proactive approach empowers healthcare teams to address potential issues before they escalate, reducing hospitalizations and improving patient outcomes.
Future trends in nursing informatics
The future of nursing informatics holds remarkable potential with advancements in artificial intelligence (AI) and predictive analytics. AI-driven algorithms can help with analyzing vast datasets to identify patterns and trends, aiding nurses in making informed decisions. Predictive analytics can anticipate patient deterioration, enabling early interventions and personalized care plans. AI bots can offer immediate answers to patient queries, enhancing communication and patient engagement while reducing the workload for non-emergencies.
Wearable devices and remote monitoring technologies are already reshaping the monitoring process of patients. Wearables can continuously gather patient data, such as vital signs and activity levels, allowing nurses to monitor patients remotely and detect changes in real-time. Improvements will continue to assist with chronic disease management, self-management of health conditions whenever possible, and reducing hospital readmissions.
In the constantly evolving healthcare industry, technology integration is not just optional. It is essential for improving care standards. The potential of nursing informatics is limitless with ongoing research and innovation. AI, wearable devices, and telehealth converge to shape a data-driven, personalized future of nursing.
More to Read:
Previous Posts: