Nurse Educators Play an Important Role in Shaping the Future of Nursing

Nurse educators play a crucial role in shaping the future of healthcare as they have direct access to new nurses coming into the field. Nurse educators are leaders in their industry and are responsible for developing nurses, promoting evidence-based practices, and fostering leadership and critical thinking. These medical professionals also shape the healthcare system by improving patient education, advancing research, and creating new and updated curriculum to teach nursing students.
Implementing policy changes
Nurse educators have a vital role in implementing policy changes within healthcare and nursing education settings. One way to influence policy change is to stay updated on current healthcare policies and regulations. They can engage in professional development activities, attend conferences, join professional organizations, and read reputable journals to stay informed about policy changes relevant to nursing education.
A good way to have an impact on future policies in nursing is to incorporate policy content into the curriculum. Nurse educators can integrate policy-related content into the nursing curriculum to ensure that future nurses have a solid understanding of healthcare policies and their implications for practice. They can develop specific courses or modules dedicated to policy education and incorporate policy discussions into clinical and classroom settings.
Engaging students in policy discussions is an excellent way to ensure that the future of nursing is being led by informed individuals who feel a responsibility to their industry. They can facilitate discussions and activities that encourage students to critically analyze healthcare policies, consider their impact on clients and communities, and examine nursing's role in policy advocacy. They can create case studies, debates, and interactive exercises that challenge students to think about policy issues and potential solutions. They can also lead by example by engaging in advocacy efforts to influence policy changes. They can write opinion pieces, publish research, and present at conferences to raise awareness and promote evidence-based policies that enhance nursing education and patient care. They can also encourage students to engage in advocacy and support their efforts in promoting policy changes.
Nurse educators can establish relationships and actively collaborate with policymakers, professional associations, and other stakeholders to contribute their expertise and insights regarding policy implementation. By participating in committees, task forces, and policy-related initiatives, nurse educators can advocate for policies that support quality nursing education and healthcare delivery.
These medical professionals can contribute to policy implementation by evaluating its outcomes and impact on nursing education and practice. They can conduct research studies, collect data, and analyze the effects of policy initiatives on student learning, program outcomes, and quality of care. This evidence can then be used to inform future policy development and implementation. They can also collaborate with peers and other educational institutions to share best practices and collectively implement policy changes. This collaboration can involve sharing resources, attending conferences or workshops, and participating in inter-institutional projects aimed at policy implementation.
Nurse educators should continuously engage in professional development to enhance their knowledge and skills in policy implementation. This can involve attending workshops or webinars, pursuing advanced degrees, participating in policy-related conferences, or joining professional organizations dedicated to nursing education and policy advocacy.
By incorporating policy content into the curriculum, engaging students in policy discussions, collaborating with policymakers and stakeholders, advocating for policy changes, evaluating outcomes, collaborating with other educators, and engaging in continuous professional development, nurse educators can effectively implement policy changes within nursing education and contribute to shaping the future of healthcare.
Developing highly-skilled nurses
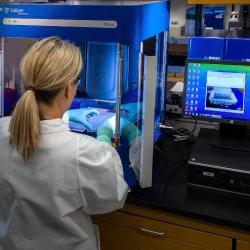
Nurse educators are responsible for training and mentoring aspiring nurses, ensuring they acquire the necessary knowledge and skills to provide high-quality patient care. By imparting evidence-based practice and clinical expertise, nurse educators contribute to the development of competent healthcare professionals. Nurse educators need to be skilled in technology and new innovations in the medical community so they can impart that knowledge to their students and ensure a bright future for nursing. These medical professionals understand that the learning never stops for educators because there are always developments happening in the medical field that need to be passed along and taught.
Promoting safe and evidence-based practice
Nurse educators emphasize the importance of evidence-based practice, ensuring that nursing interventions are based on the best available research. They educate nurses on the latest advancements in healthcare, promoting efficient and safe care delivery. This type of training includes innovations in technology such as software programs that keep track of patient’s medical records and other tools that make a nurse’s life easier during their busy day. Safe practices include keeping confidential records safe and ensuring that the whole medical team has access to the same medical records. By promoting and training new nurses in these types of practices, nurse educators can ensure that future leaders in the industry will be knowledgeable and able to provide excellent patient care.
Fostering leadership and critical thinking skills
Nurse educators help cultivate leadership qualities and critical thinking skills among nursing students. This equips nurses to make sound decisions in complex and rapidly-evolving healthcare environments, ultimately improving patient outcomes. Nurse educators act as mentors to new nurses and support them when tough decisions need to be made or a problem needs to be solved. These medical professionals can help nurses gain confidence and good judgment by teaching them how to make objective decisions based on medical evidence. The confidence this builds helps improve the overall atmosphere of the nursing department and gives those nurses who are ambitious a chance to practice their leadership skills.
Leadership and critical thinking are two areas that an individual can develop while applying to participate in the master of nursing education online programs at an accredited school like Cleveland State University. The programs for nursing leaders will teach individuals how to train new nurses, create engaging and sound curricula, and acquire the teaching skills they need for a successful career.
Improving patient education
Through their work, nurse educators enhance patient education by developing teaching strategies and materials that support effective communication between nurses and patients. By empowering patients with knowledge about their health conditions, nurse educators contribute to better self-management of diseases and improved overall health outcomes. Nurse educators also teach new nurses how to focus on patient-centered care and create a collaborative relationship with their patients. This holistic approach to healthcare means that everyone on the medical team, including the patient, is involved in making decisions that are practical and possible for the patient.
Nurse educators play a vital role in improving patient education through their instruction by equipping future nurses with the necessary knowledge and skills to effectively educate patients. One way for nurse educators to contribute to enhancing patient education is to train students in effective communication techniques, such as active listening, empathy, and clear and concise explanations. These skills enable nurses to establish rapport with patients, understand their needs, and provide them with accurate and understandable health information.
Nurse educators educate students about health literacy concepts and strategies. They teach nurses how to assess patients' health literacy levels and tailor education materials accordingly, using plain language, visual aids, and audiovisual resources to improve patient comprehension and engagement. These leaders also promote cultural sensitivity and awareness among students. They teach future nurses to recognize and respect diverse cultural beliefs, practices, and languages, ensuring that patient education materials and approaches are appropriate and meaningful for different populations.
Nurse educators emphasize the importance of health promotion and disease prevention during patient education. They teach students about lifestyle modifications, preventive screenings, immunizations, and early detection strategies, enabling nurses to empower patients to take an active role in maintaining their health. They also encourage student nurses to adopt patient-centered teaching methods, which focus on individualizing education based on patients' preferences, needs, and learning styles. They teach strategies for collaborative goal setting, involving patients in decision-making processes, and providing ongoing support and follow-up.
Educators in nursing train students in shared decision-making models, facilitating open dialogues between patients and healthcare providers. They emphasize the importance of providing patients with accurate and evidence-based information to help them make informed choices about their care. They also incorporate technology and multimedia resources into their instruction to enhance patient education. They teach students how to use health-related applications, interactive websites, videos, and mobile health tools to deliver engaging and accessible education to patients.
These medical professionals foster interprofessional collaboration among students, teaching them the importance of teamwork and the benefits of interdisciplinary approaches to patient education. They emphasize the role of nurses in working collaboratively with other healthcare professionals to provide comprehensive and holistic patient education. By equipping future nurses with effective communication skills, cultural sensitivity, health literacy knowledge, patient-centered teaching methods, shared decision-making approaches, technology integration, and interprofessional collaboration, nurse educators contribute to enhancing patient education and promoting better health outcomes.
Advancing nursing research and evidence
Nurse educators are actively engaged in nursing research, contributing to the body of knowledge that underpins evidence-based practice. Their research efforts lead to innovations in care delivery, improved patient outcomes, and advancements in the nursing profession. By training new nurses on research opportunities and the latest innovations in the profession, these medical professionals provide an exciting look into the innovations in healthcare and how these advancements help improve the nursing profession.
Creating the curriculum for new nurses
Nurse educators follow a system when they create a new curriculum that starts by identifying the educational needs of learners and the healthcare system. They may conduct surveys, hold discussions with stakeholders, review industry trends, and analyze data to determine the knowledge and skills required by nurses in their specific practice areas.
Based on the needs assessment, nurse educators define clear and specific learning outcomes. These outcomes should align with the desired competencies and goals of the program or course. Learning outcomes provide a framework for designing the curriculum.
Nurse educators then identify the content that needs to be covered to achieve the desired learning outcomes. They consider relevant theories, evidence-based practices, guidelines, and standards of care. They also consider the specific needs of the target learners, ensuring the curriculum is tailored to their level of education and experience.
These medical professionals determine the teaching methodologies and educational strategies that will be employed to facilitate learning. This may include lectures, simulations, case studies, hands-on practice, group discussions, online resources, and clinical experiences. They apply educational principles and best practices to ensure the effective delivery of the curriculum.
Nurse educators develop various assessment methods to evaluate learners' progress and achievement of the learning outcomes. This may include written exams, practical demonstrations, clinical evaluations, research projects, and reflective portfolios. Assessment methods should align with the learning outcomes and provide feedback to learners. They also consider the use of technology and educational resources to enhance the curriculum. This includes integrating multimedia materials, virtual simulations, computer-based learning tools, and interactive online platforms. They ensure access to up-to-date resources that support effective and engaging learning experiences.
Leaders in nursing education regularly evaluate the curriculum's effectiveness and make revisions based on feedback, learner performance data, and emerging trends in healthcare. This continuous evaluation and improvement process ensures that the curriculum remains relevant, current, and aligned with the evolving needs of the healthcare system. Throughout these steps, nurse educators collaborate with colleagues, industry experts, and other stakeholders to create a comprehensive, evidence-based curriculum that prepares nurses for their roles in healthcare delivery.
Skills needed to be an effective nurse educator
These medical professionals need clinical expertise to have the knowledge to teach others. They should have a strong background and extensive knowledge in various clinical areas of nursing practice. This expertise allows them to effectively teach and guide students in real-world patient care scenarios.
Nursing educators should have the ability to teach others. A nursing leader needs to be able to show new nurses medical methods and theory with patience and discipline in a way that the individual will respond to. They must possess excellent teaching skills to effectively communicate information, engage learners, and facilitate effective learning experiences. They need to be able to adapt their teaching methods to accommodate different learners and create a positive and inclusive learning environment. This includes understanding their students as individuals and developing a mentor-mentee relationship.
Nurse educators should have excellent verbal and written communication skills to effectively convey complex nursing concepts and theories. They need to be able to explain information clearly, actively listen to students, and provide constructive feedback.
Critical thinking is an important skill for nurse educators to possess and teach to new nurses. Strong critical thinking skills help students analyze and solve complex healthcare problems. They should be able to encourage and guide learners to think critically and apply evidence-based practice in their decision-making.
A nurse educator should be skilled at developing curriculum that teaches new nurses the basics of the job as well as new techniques and innovations that they will need to know about for the future. They are often responsible for developing and updating nursing curricula to ensure it aligns with current best practices and emerging trends in healthcare. They should be knowledgeable about curriculum development principles and possess the ability to create engaging and relevant educational materials. This skill includes the knowledge that the program is constantly in flux and their role as educators means they also need to be learning constantly and keeping up with the latest in healthcare.
Educators often play a leadership role within their academic institutions. They need to effectively manage and coordinate educational programs, mentor and support students, collaborate with colleagues, and participate in professional development activities. As technology becomes more integrated into healthcare and education, nurse educators should be comfortable using various digital tools, such as learning management systems, simulation software, and telehealth platforms. They should also be familiar with online teaching methods and remote learning techniques. They need to adapt to evolving healthcare practices and pedagogical approaches. It’s important that they continuously update their knowledge and skills to stay current with advancements in nursing education and practice.
Conclusion
Nurse educators are crucial to the development and enhancement of the nursing profession by teaching new nurses the skills necessary to provide excellent patient-centered care. By engaging students and emphasizing the importance of advocating for their patients as well as their industry, nurse educators are the first exposure students have to the challenging and rewarding career of nursing.
More to Read:
Previous Posts: