A Nurse’s Role in Patient Safety and Quality of Care

One of the most important duties within the nursing profession is to protect patient safety at all times. This basically means avoiding “preventable harm” while an individual is in their care. The harm could be from many different risks. The most obvious is a deterioration in a patient’s health that goes undetected. However, preventable harm could also be a wide range of other issues with equipment, medication, and the actions (or oversights) of other healthcare staff. Even the simple act of cleansing hands, equipment, and surfaces properly and regularly is an element of a nurse’s duty of care, as cross-contamination is a constant threat to patient safety.
According to the CDC (Centers for Disease Control and Prevention), each day, 1 in every 31 hospital patients develops a new infection while being treated in a medical facility. That can include being infected by antibiotic-resistant bacteria that could prove fatal, especially if your health or age already makes you vulnerable. Healthcare-associated infections (HAI) are believed to cost US hospitals at least $28.4 billion a year.
The need to monitor and protect patient safety as a nurse naturally also makes it essential for them to be highly focused on care quality standards. Nurses in all job roles must work to provide the best possible healthcare experience and outcomes for their patients.
In effect, that can mean becoming the patient’s advocate, particularly in hospitals and trauma situations when individuals can be in highly vulnerable positions. Vulnerable patients could lack even the most fundamental abilities to care for themselves or properly communicate their needs. This puts the focus on nursing professionals to ensure that nothing is overlooked or left to chance, ensuring patients are protected from the multitude of risks and ever-present preventable harms.
It can be a matter of life and death
The possibility of a patient developing an HAI while in your care is just one of the potentially life-threatening risks that nurses must work hard to avoid. Every year, figures are published highlighting not just patient deaths but also those attributable to medical neglect or mistakes. Clearly, every nurse seeks to keep both of those statistics as low as possible by championing healthcare quality standards.
However, quality of care in nursing extends far beyond facts about mortality. This is a profession with a long history of protecting patient experience too. Nurses seek to ensure that every individual in their care is kept comfortable and feels positive and heard.
This is why nursing is considered to be the most trusted and respected profession globally. Professionals in this field are known for delivering patience, empathy, and compassion in often distressing situations.
Training and the responsibility of nurses
Patient safety is a highly complex topic. For instance, in a healthcare situation, not doing something right, not doing anything at all, or doing too much of something can all have serious repercussions. Also, the smallest of details can take on huge significance in healthcare situations, from how well nurses wash their hands, to how accurately they act on a physician’s treatment instructions. That is why the amount of training nurses now need is so intensive and extensive. They have a lot of professional and personal skills that they need to apply while providing every patient with responsive, appropriate, and successful care.
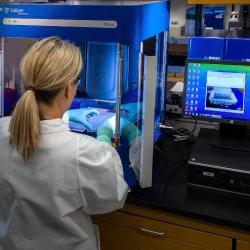
This is why Elmhurst University’s online nursing program offers a robust blend of 100% online coursework, with access to its state-of-the-art Simulation Lab, as well as one or two on-campus residencies, and clinical placements in the learner’s local community. It is a combination that gives every nurse graduate a strong appreciation of the realities of patient care. Experience, technical study, and personal development all contribute to a nurse’s ability to evaluate situations swiftly and act decisively to keep patients safe and on their way to positive outcomes.
Omissions and treatment accuracy
One of the first things nurses learn to do is to develop an open and honest relationship with their patients. That goes alongside being able to systematically ask a series of essential questions in a thorough and diligent manner. This is the bedrock of a nurse’s work to gather and record important patient histories. Having digital medical records to rely on is a big step forward, but it can still be greatly enhanced by anecdotal information that the nurse gathers.
For example, a patient’s recent overseas travel or current living conditions could prove to be an essential detail that the physician needs to know so they can make an accurate diagnosis. The wrong diagnosis can lead not just to ineffectual treatment but also to a potential worsening of an undetected medical condition. Nor does this important patient dialogue and observation end when medical history is used to help create a diagnosis. Nurses are also responsible for a wide range of monitoring and evaluation tasks as a patient’s treatment progresses. They are the healthcare professionals who are best placed to spot issues and anomalies quickly.
Examples of this could be a nurse who becomes concerned a patient is not responding well to a particular drug, including experiencing slow healing or noticeable side effects. When the nurse updates healthcare colleagues, it could be that a change in medication sets the patient on a far more positive track.
This constant monitoring of a patient’s condition is especially crucial for factors that cannot be measured by even the most advanced medical technology. For instance, if a patient starts to have sudden difficulty speaking, seeing, or walking, or shows facial weakness, it can be a warning sign that they are having a stroke. A fast-thinking and acting nurse can ensure that this early warning sign is not overlooked, leaving the patient at risk of permanent brain injury, disability, or even death.
Medical technology and patient safety
It could be safely argued that medical technology (MedTech) has gone a long way toward improving patient safety. This in turn relieves some of the heavy duty of care traditionally carried by nurses. For example, there is now drug dispensing equipment that automates both timing and dosage. This equipment runs alongside a plethora of devices to accurately measure vital signs and other medical information, which greatly mitigates opportunities for error or oversight by medical team members.
However, there is still a big emphasis on nursing instinct and interaction with patients. Especially as each patient has their individual needs and experiences, medical data and equipment readings cannot replace the relationship nurses have with their patients.
It is also often a nurse’s responsibility to know when and how to use the technology that supports their everyday tasks and aims.
Communication and protecting patient safety
One of the responsibilities nurses have to uphold patient safety is being ready to flag up their concerns quickly with a more senior member of the healthcare team, or indeed with their human resources department. That could be concerns about malfunctioning equipment, a worry about the accuracy of treatment protocols, or indeed a fear that a colleague is acting inappropriately.
Another communications task that falls within the nurse’s duty of care is keeping accurate patient records, but also providing detailed information and insights (or listening carefully) during shift handovers and patient transfers.
Good communication by nurses also revolves around speaking up when they feel patient care is inadequate. They need to be ready to consult colleagues, clinicians, and family members when the situation demands it, and when patient safety or general care is at risk.
Other risks to patient safety
This article has already mentioned some of the preventable harms that can put patient safety at risk, including errors with medication and equipment, healthcare-associated infections, and diagnostic mistakes. However, there are other, more fundamental quality issues that can put patients at risk, particularly those who are elderly, frail, or largely confined to their beds.
For instance, unconscious or generally immobile patients must be moved regularly in the beds and chairs and must have regular checks for pressure sores. When not carefully managed, pressure sores can become infected, adding to the patient’s risk of serious harm. Also, patients in hospitals, clinics, and community settings need to be evaluated and monitored for their risk of falling. A nurse may be the health or social care professional who is tasked with finding aids or methods that avoid the patient taking a tumble, without stripping them of their independence and dignity.
Patient care can also incorporate making sure that patient mental health is being properly respected and observed. That could include completing basic tasks to make patients feel fresh and comfortable in a hospital setting or providing support and encouragement as a key element of holistic nursing care.
Another illustration of the safety issues nurses need to be aware of is deep vein thrombosis and pulmonary embolism (DVT/PE). These are the types of blood clots that can form in a patient who is confined to bed, or who has recently been injured or is recovering from a surgical procedure. Even the cast on a broken limb has the potential to lead to a dangerous blood clot forming. Such things as a family history of blood clots, cancer treatment, and inflammatory bowel disease can increase a patient’s risk of DVT.
Nurses need to be especially aware of the potential for this issue to arise, as over 50% of patients who get these blood clots have no discernible symptoms. Nurses must be ready to conduct physical examinations for such symptoms as redness, swelling, pain, and tenderness. Symptoms of a pulmonary embolism include breathing issues, a faster-than-usual or irregular heartbeat, and very low blood pressure.
Clearly, the “little things” can matter in nursing, and a professional who cares about patient safety must be constantly alert and conscientious of patient health.
Creating a culture of quality care
As advanced nursing professionals are often in leadership roles, another aspect of their work to protect patient safety is working with colleagues to promote their commitment to the highest possible standards of care.
The American Nurses Association lists the key components of a culture of safety and defines it as “Core values and behaviors resulting from a collective and sustained commitment by organizational leadership, managers, and health care workers to emphasize safety over competing goals.”
What that amounts to is making sure that everyone in your team understands their roles and responsibilities with regard to patient safety. It can also involve providing additional training and coaching to reinforce safety values and quality standards.
One of the most vital elements of a culture of quality care is systems that help staff learn from errors and oversights. Professional misconduct is a separate issue, but many of the “learning situations” are relatively small-scale infringements of a healthcare provider’s policies and procedures. Rather than creating a culture of blame and shame, a lead nurse could bring about quality improvements by making their colleagues aware of the improvements they can make.
This situation also requires other leadership skills for nursing professionals. For example, they need emotional intelligence and the ability to spot when colleagues are tired, in a low mood, or feeling overwhelmed. These are the times when mistakes and oversights become far more likely.
Future demands on responsible nursing
Health information technology (HIT) has greatly improved the work nursing professionals do in recording patient information and communicating and collaborating with colleagues. Thanks to HIT, it is now possible to share detailed medical data—including scans and other imagery—in real-time with medical professionals at different locations around the world. The duty of care this brings clearly involves keeping digital records up to date but also taking steps to keep sensitive medical information private and secure. This is a quality and safety issue that is growing as technology makes it increasingly possible to support telemedicine.
Patients can wear devices that monitor key health factors or go about their normal lives with internal medical devices that monitor or support bodily functions. From a remote location, physicians and nurses can regularly evaluate this information and act quickly when they spot an anomaly or escalating issue. Or the patient can request a medical appointment online. It is vital that anyone operating healthcare services of this kind knows how to secure a remote medical practice, keeping patient confidentiality as a high priority at all times.
However, the nurses within the team will also have to develop the ability to maintain quality of care, and protect patient safety, within the perimeters of this “hands-off’ situation”. For instance, when conducting remote appointments, with no opportunity to examine the patient in person, and limited ability to read non-verbal cues such as body language—a nurse may well have to ask far more questions to generate vital feedback from the patient. They may also have to act quickly and decisively on even the slightest suggestion that a patient is facing a medical issue.
How nurses lead global trends
Responding to transformation in the healthcare sector is just one of the ways that nursing professionals are at the forefront of innovation and change. They also influence other developments in the way patient safety is protected, and the manner in which quality standards continue to improve.
Examples of this include the role nurses play in gathering best practice insights, and evidence-based suggestions. They serve on hospital committees and boards to bring about change, and lobby and campaign at the state and national levels to bring about improvements in patient care.
Larger healthcare providers sometimes employ well-qualified and experienced nurses to lend their unique insights to make the whole organization more accountable and effective in the quality of care. This includes posts as “quality improvement management nurse”.
This role would include ensuring their employer remains compliant with legislation but also making sure that the organization is 100% committed to improving patient outcomes and experiences and has clear and achievable goals with regard to quality.
Conclusion
There are numerous ways that the work of nurses improves healthcare quality and patient safety. By taking on board the information in this article and gaining the relevant qualifications, you can soon be working in a rewarding nursing role in which you play a key part in the health and well-being of your community.
More to Read:
Previous Posts: