Reasons To Use A Clinical Documentation Improvement (CDI) Program
As healthcare organizations expand their use of electronic health record (EHR) data for a variety of use cases and clinician burden issues increase, there has been an increased emphasis on enhancing outpatient CDI.
In a recent survey, it was observed that 36% of clinicians spend more than half their day on administrative duties in the EHR. Also, 72% of doctors anticipate spending more time on paperwork in the coming year.
Clinical Documentation Improvement (CDI): An Overview
The documentation must always be full, clear, dependable, and consistent in order to reap the benefits. Moreover, a clinical documentation integrity program aids in the conversion of clinical data from paper to code in order to better represent a patient's clinical data.
The information is then incorporated into various databases, such as those tracking public health and the performance of individual doctors. The information provided by clinical documents (CDI) has a significant effect on patient treatment and is invaluable to the team. Standardizing and accelerating processes in patient care and daily operations is the goal of CDI.
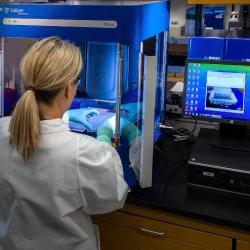
Doctors that take notes are part of a healthier care community because they improve communication within their offices. Some hospitals and clinics have already begun to implement automated technologies to enhance clinical notes.
Here are the top seven reasons for sticking to a successful CDI procedure:
1. Compliance
The medical community uses it frequently. Healthcare executives have serious worries about noncompliance and will often go to great lengths to make sure it is addressed. Better compliance can be achieved in your hospital with relatively little effort by implementing a solid CDI program.
False audits, penalties, and expensive corrective actions can result from a lack of proper, timely, and accurate recordkeeping. CDI enables the development and reporting of information that is not just real-time but up to the mark, clear and detailed.
2. Reduced Claim Denials
There are many grounds on which an insurance company can reject a patient's request for medical treatment. Insurers may deny payment for medical care if a claim is sent after the deadline has passed, is incomplete, or contains errors. A patient's claim is less likely to be denied if they work with a professional CDI who makes sure their claims are complete, understandable, and filed on time.
3. Improved Quality Patient Care
Incorporating CDI can be challenging, depending on the available workforce. However, when you mandate expert CDI services for selected employees, everyone can concentrate on what they do best while documentation errors are reduced. Hence, healthcare professionals offer clinical documentation enhancement services to enhance patient records and guarantee accurate data reflecting diagnosis and treatments.
4. Streamlined clinician engagement
There are many benefits to having increased doctor participation in hospital operations. Among these are compliance, patient security, and data integrity. Data integration provides two benefits immediately upon implementation: real-time reporting and the ability to share data in real time. In what way? Better patient outcomes and increased transparency in operations. As the CDI takes effect and you start receiving data in a finer grain, your clinicians will be able to take in more information in less time, freeing them up to focus on what really matters: the patients.
5. Improved or more accurate patient data
Accurately recording and tracking patient information benefits, not just the patient but also the healthcare providers, insurance companies, and anybody else who has access to the patient's medical history. By adopting CDI, healthcare providers and payers will share consistent information about a patient's condition and treatment.
6. Decreased Physician Queries
Doctors understand that the way they communicate and write has an impact on things like billing and quality metrics. Coders are responsible for examining physician notes and assigning CPT and ICD codes based on the information found therein. If the patient's records are unclear or contradictory, coders will contact the doctor to get more information. Complete, legible, and error-free clinical documentation is more likely with expert CDI support.
7. Enables Greater Access to EHRs
It is obvious that doctors sometimes make mistakes while handling paperwork. Patients who study their own medical records may discover inaccuracies that prevent them from receiving the best possible care. Patients can check their health records and make any changes.
What Kind Of CDI Guidance Is Available To Providers?
For accurate documentation throughout the whole patient record, AHIMA launched two CDI toolkits in 2018. The first addresses outpatient documentation and the second is dedicated to denials management.
As clinicians increasingly rely on coded data, proper documentation is more important than ever. There is a genuine need for that additional degree of specificity in the documentation process, which is why provider education is crucial with CDI.
To guarantee high-quality data for patient care, quality reporting, and other applications in the healthcare industry, CDI health IT will continue to be used as the digital health transition advances.
The Role Of CDI In Transforming Healthcare Services
According to a detailed study published in 2016 by the American Medical Association (AMA), medical professionals spend 30 minutes per hour on average with patients and another 30 minutes per hour on electronic health record (EHR) documentation. Only about a quarter of their time is spent really caring for the patient, while the remaining half is spent documenting their care in an electronic health record.
The organizations need to assess how well they are doing with clinical documentation and the revenue cycle now. To do this, they must determine which hierarchical condition categories and critical quality measurements have inadequate documentation. When professionals are aware of the voids, they can direct their attention to the programs most likely to generate income.
Certified Clinical Documentation Specialists and Clinical Documentation Improvement Practitioners are required members of the CDI team. It is up to the leaders to decide if the use of automated documentation is necessary.
Conclusion
To sum up, CDI can become an invaluable ally. If your organization is interested in increasing revenue and improving the quality of care for your patients, high-value clinical decision support (CDS) program may be the way to go. Improving your clinical documentation will become increasingly important as time goes on, and maybe the deciding factor between your hospital being an efficient system that prioritizes patient care and another hospital failing to keep up with the times.
More to Read:
Previous Posts: