Sterilization of Dental Instruments

Sterilization of Dental Instruments
Everyone knows that medical or dental instruments need to be clean. But do they need to be sterilized? If you are working on a medical clinic construction, you might want to plan an extra space for sterilization. Here, you will get a chance to discover the benefits of equipment sterilization and see why this process is crucial for every dental office. We will also help you understand how to plan properly for medical center interior design to ensure that you have everything you need to start your business.
The Importance of Proper Sterilization of Dental Instruments
The first thing we will need to address is the importance of proper sterilization of dental instruments. Having sterile and disinfected instruments as a dentist is the key to making sure your patients are safe. It should be an essential part of your everyday routine, and you should do everything in your power to ensure that your equipment is safe to use at all times.
The primary reason why this is so important is that it saves both the workers and patients from infections and unnecessary diseases. We all know that dentists work on our teeth. But what is important here is that the bacteria and viruses from the mouth can transfer to instruments: hepatitis, herpes, COVID-19, the list goes on.
Since the dentist and staff will be in contact with instruments and equipment, it is more than easy to get infected without proper care. Sterilizing and sanitizing everything minimizes the risk. That is why you need to know how to properly clean your office before the next patient arrives.
Categories of Dental Instruments
Not every instrument needs identical care. Some are used more than others, and there are different categories of dental instruments. Based on the Centers for Disease Control and Prevention, there are three categories of dental instruments. They are classified as critical, semi-critical, and non-critical.
Critical Instruments
Critical instruments are those used to penetrate bone or soft tissue during a dental procedure. For this category, instruments need to be sterilized after each use. There are a couple of different ways to sterilize them, and we will cover them all in a bit. Keep in mind that critical instruments need to be heat resistant too, so if you own something that can’t be heat sterilized, you should replace it as soon as possible.
These instruments include scalpels, forceps, scalers, bone chisels, burs, and many others.
Semi-Critical Instruments
Semi-critical instruments don’t penetrate either bone or soft tissue, but they are in contact with oral tissues. The most common examples include, for example, mirrors. These instruments are also at risk of spreading a disease, which means that you should sterilize them after each use as well.
In some cases, sterilization might not be feasible, and disinfection will be enough.
Non-Critical Instruments
These instruments get in touch with skin, but only if it is intact. And they are not in contact with mucous membranes. That means that they don’t require sterilization, and in the majority of cases, low-level (or intermediate) disinfection will be enough.
Examples of non-critical instruments are external components of x-ray heads, blood pressure cuffs, and others.
Types of Sterilization
Depending on the instruments you need, you will pick one of the three sterilization options. They are all common in dental offices, and they all have their own purpose:
- Steam sterilization - The first method is steam sterilization, also known as an autoclave. The idea behind it is quite simple: each item is placed in contact with steam at a specific pressure and temperature and for the time needed to kill all microorganisms. Steam sterilization can reach between 250 and 273 degrees Fahrenheit (between 121 and 134 degrees Celsius). The time for sterilization can vary between four and twenty minutes, based on the instrument.
- Dry heat sterilization - Here, we use either forced or static air. With forced air, the air is heated, and it circulates through the oven. As for the static air, the temperature is increased until the air starts to rise. To achieve sterilization, the air is heated between 300 and 375 degrees Fahrenheit (which is between 150 and 190 degrees Celsius)
- Unsaturated chemical vapor - This process uses a combination of alcohol, acetone, formaldehyde, ketone, and water. It will create vapor that will be able to sterilize instruments. The process requires high pressure, time, and increased temperature (around 270 degrees Fahrenheit).
Each of these methods can be effective, and it will allow you to sterilize instruments in your office. And as you could have seen from the list, the instruments need to be heat resistant since all of these methods include high temperatures.
Steps in Sterilization of Dental Instruments
There are three main steps you will need to follow during the sterilization procedure. The only way to sterilize instruments is if they are clean. But the first step is preparation. It is important to ensure that you and your staff are safe during the process. There is a reason safety equipment exists, and it is highly recommended to use safety glasses, masks, and gloves to eliminate the possibility of spreading germs. Once you are sure that you and your staff are safe, you can proceed.
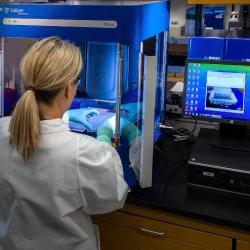
There are many different ways to clean instruments. You can try out ultrasonic cleaning, and soundwaves will help get rid of visible debris from the dental instruments. You can also use automatic washers and even scrub them manually. Once the instruments are clean, you can proceed to the sterilization process, but be sure to avoid contaminating instruments once you have scrubbed them potless.
The final step of the process is sterilization, and you can use any of the methods we mentioned. The only thing left to do once the process is over is to store the instruments somewhere safe. They need to be in a dry and protected area, ensuring that they won’t get contaminated or exposed to anything until you are ready to use them.
More to Read:
Previous Posts: